Project Name:
Theia
Country:
World
Agency:
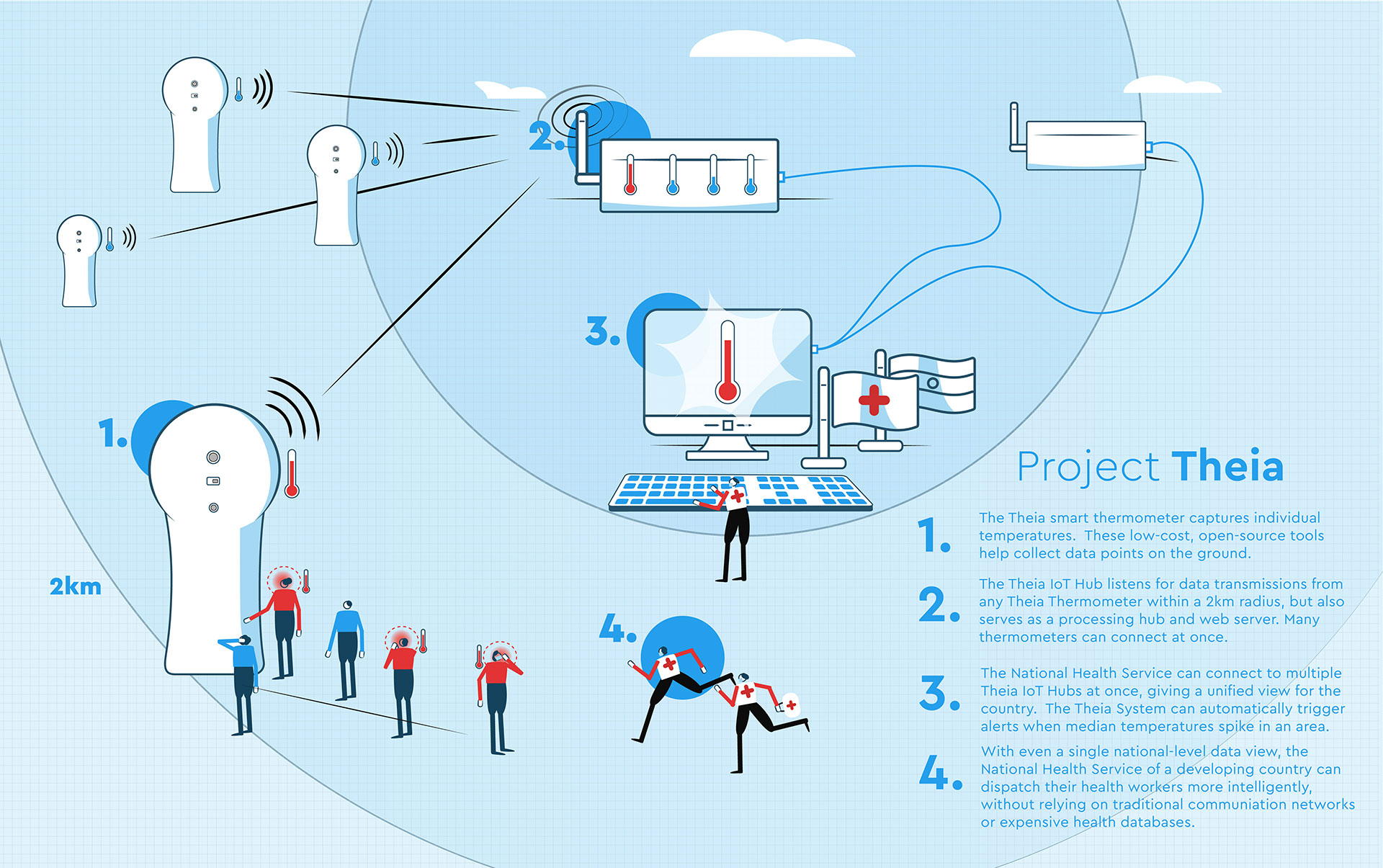
Project Theia is a low-cost platform which uses clinical sensors and ultra-long distance IoT radios to create an emergency real-time health data layer in developing countries, routing health workers where they are most needed to combat the spread of COVID-19.
Winner of the UN Development Program's 'Global COVID-19 Detect and Protect' Innovation Challenge.
The platform offers developing countries with minimal healthcare infrastructure and disrupted (or substandard) telecommunications networks a limited real-time health data layer, which allows them more effectively triage the pandemic at a national level.
Unfortunately, often the developing countries with limited healthcare systems are also those with the least real-time health data, which could otherwise be used to direct even modest services where they are most needed.
To address this, Theia collects real-time, on-the-ground contactless body temperature information. It sends the data to independent self-hosting data collection Hubs using ultra-long-distance IoT radios. The collected data is interpreted, analyzed, and served by the Hub (or multiple hubs), giving countries a functional, abet limited, real-time emergency health data layer to more intelligently deploy their health services more effectively than before.
Theia Thermometer:

The Theia Thermometer is the most visible and on-the-ground aspect of Theia. It not only collects raw datapoints of individual temperatures in a community but also operates as a fully functional high accuracy contactless thermometer. This low-cost, entirely open-source, contactless thermometer incorporates multiple temperatures sensors to ensure accuracy and ease of manufacture on the ground in developing countries. While a fever is not indicative of COVID-19, with several unrelated reasons that a person might have a heightened body temperature, there are psychological group benefits to checking for elevated temperatures of those going in and out of public markets, government buildings, and meeting areas.

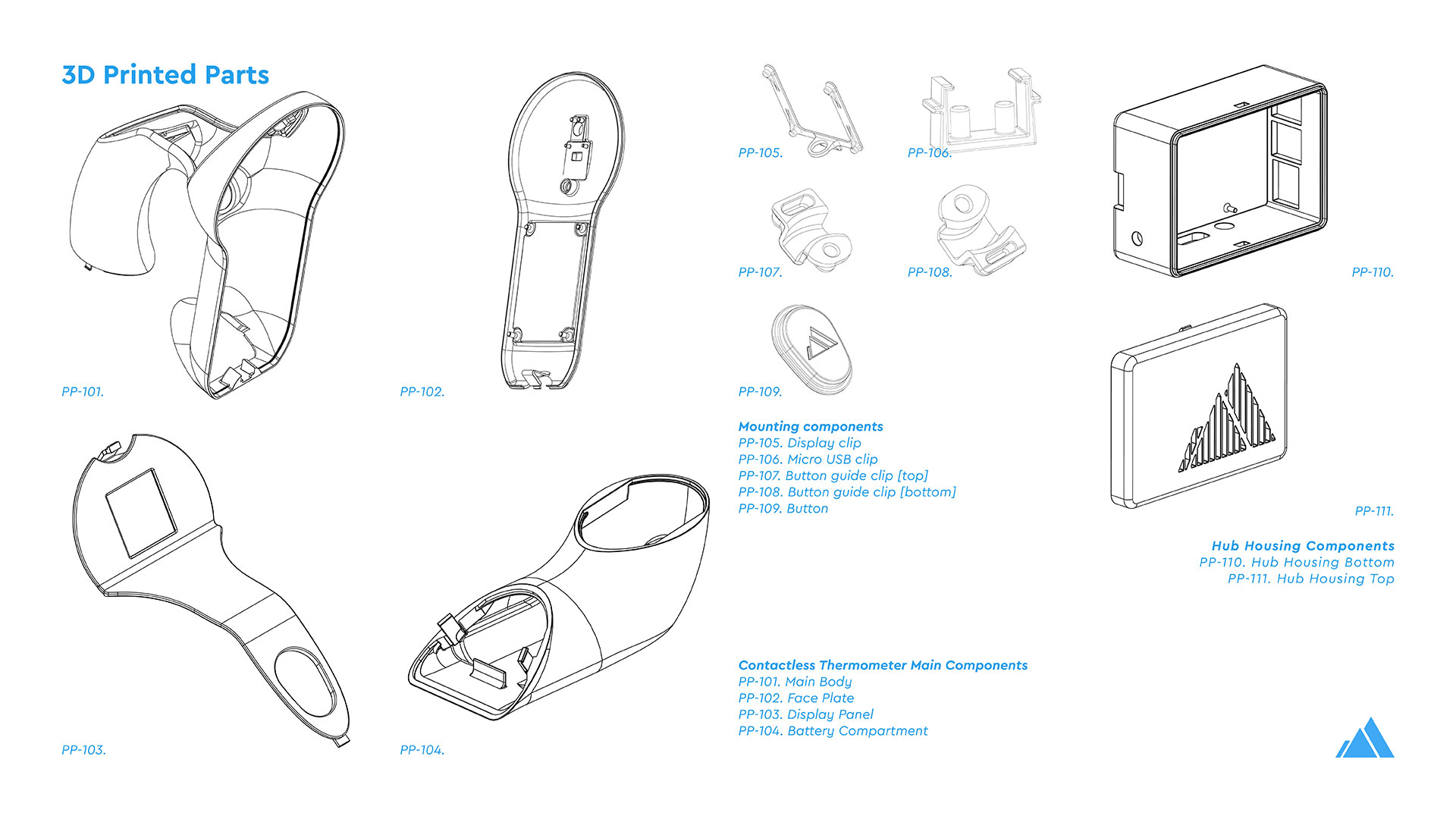
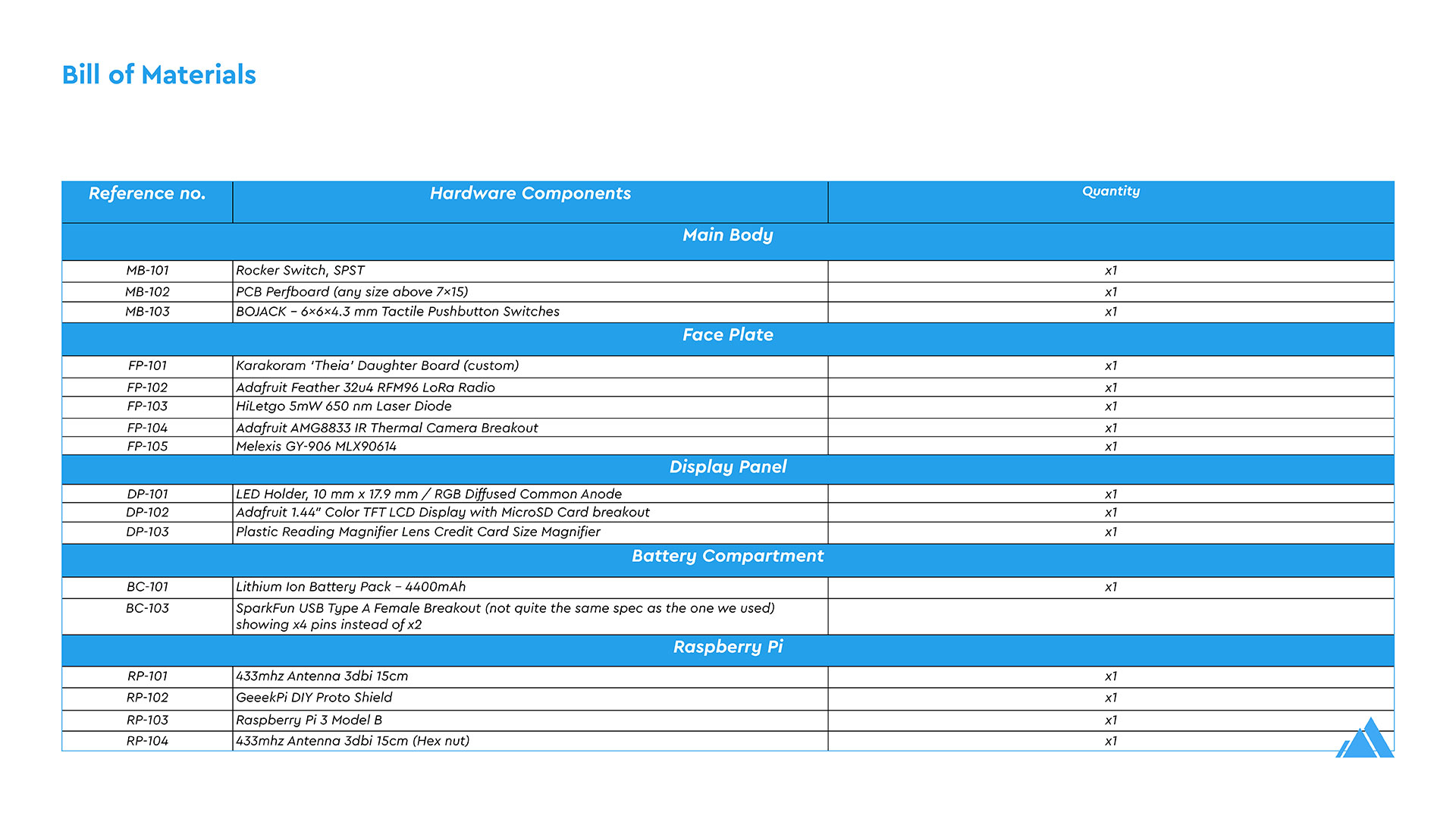
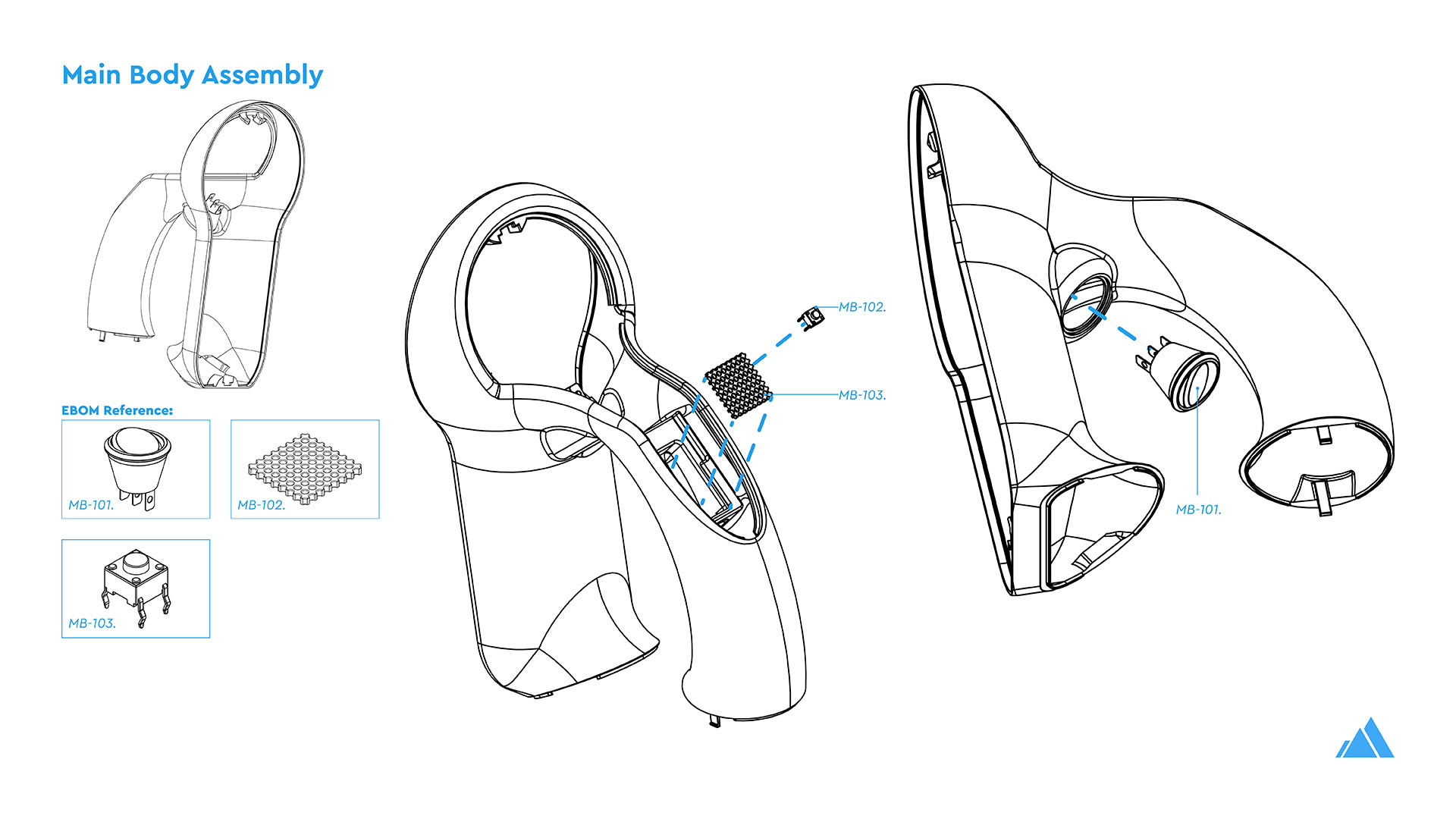
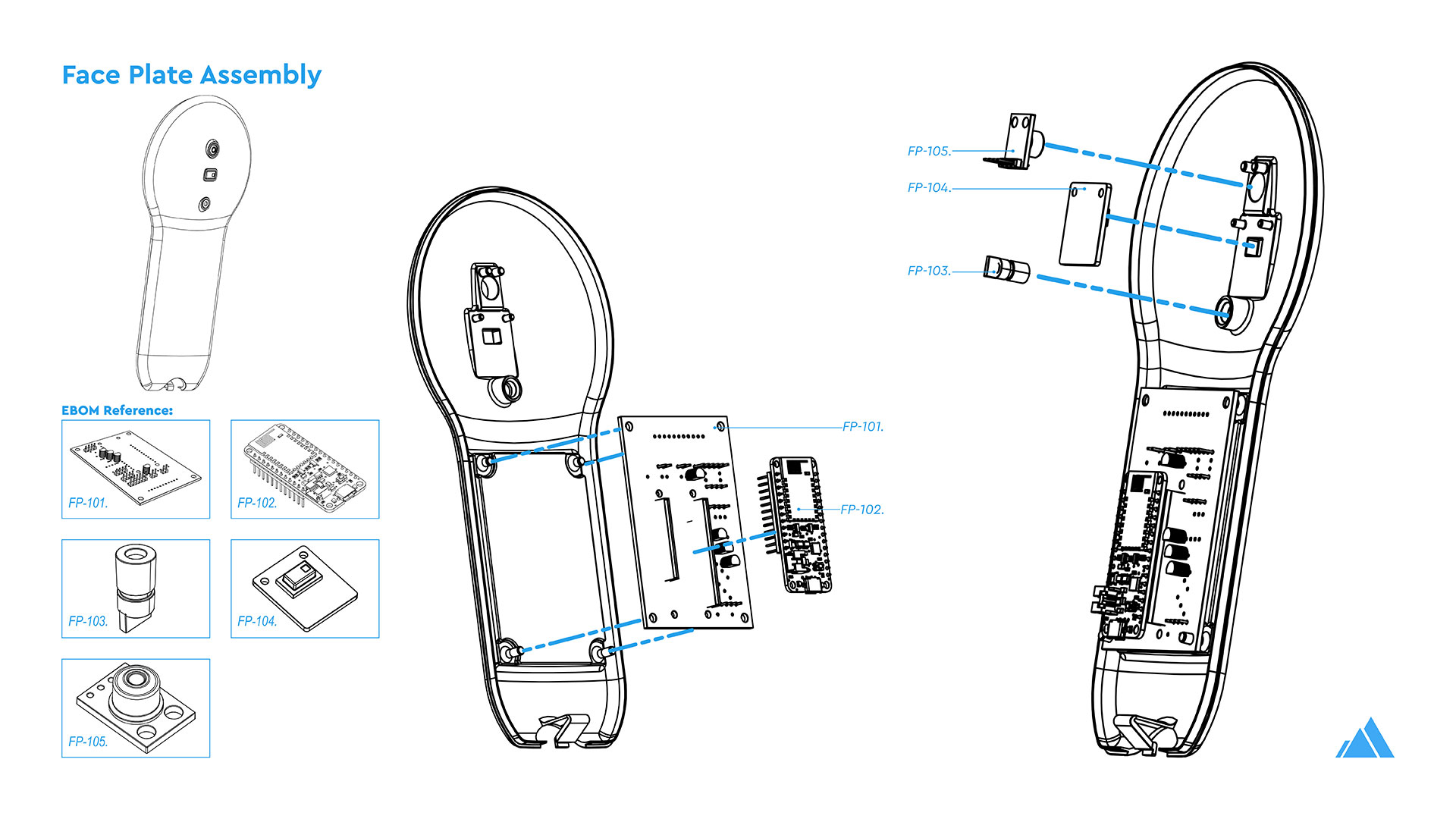
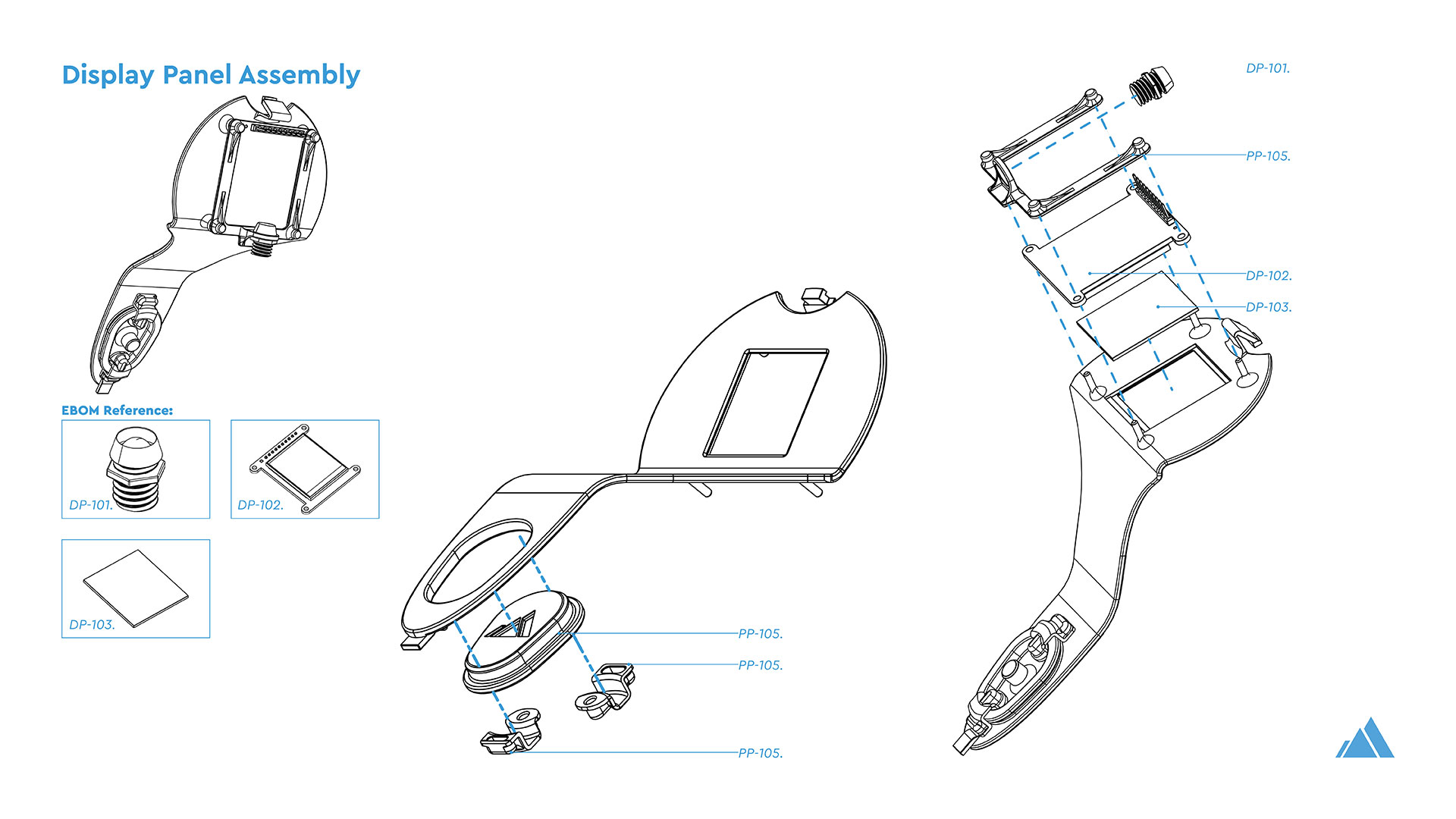
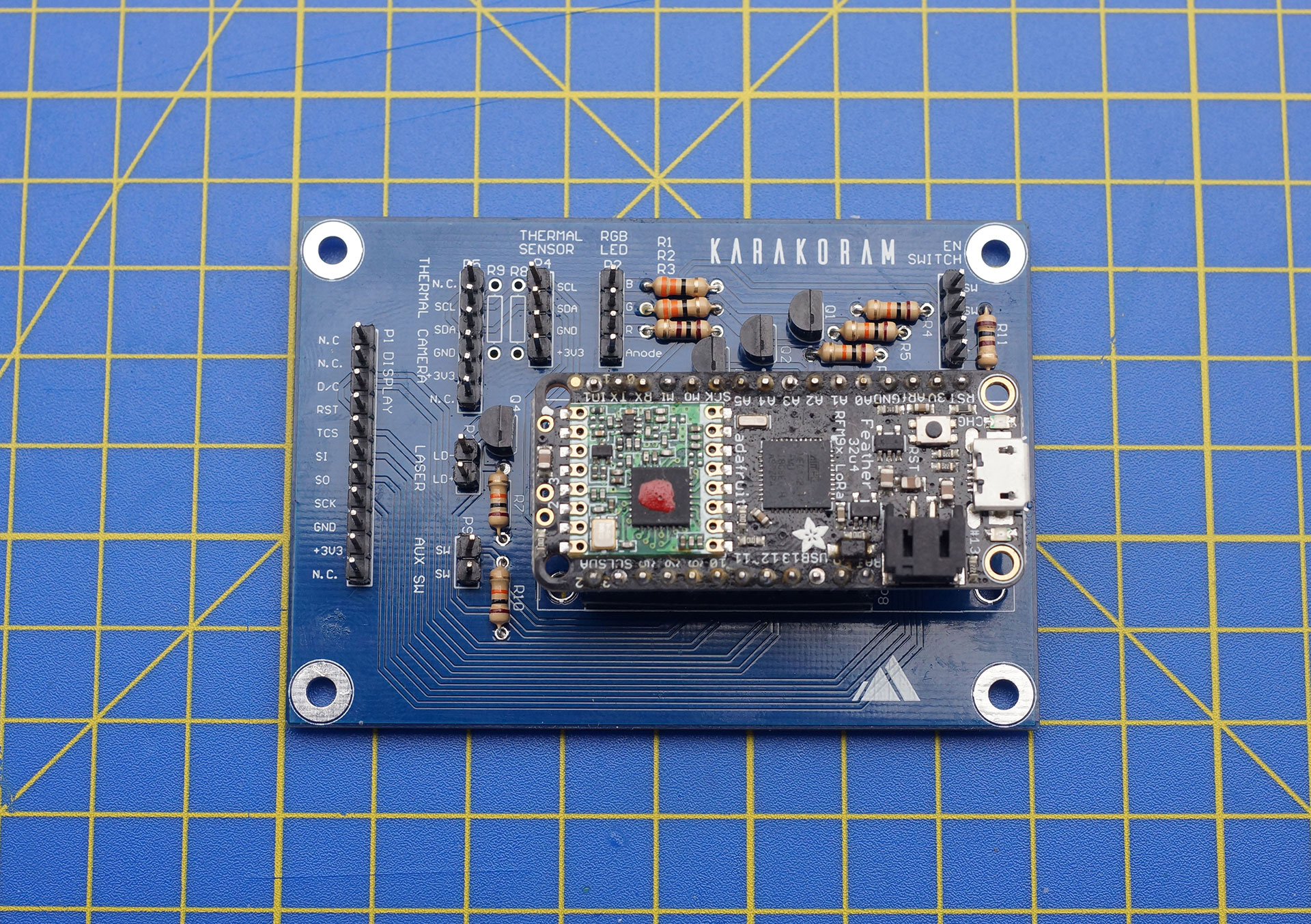
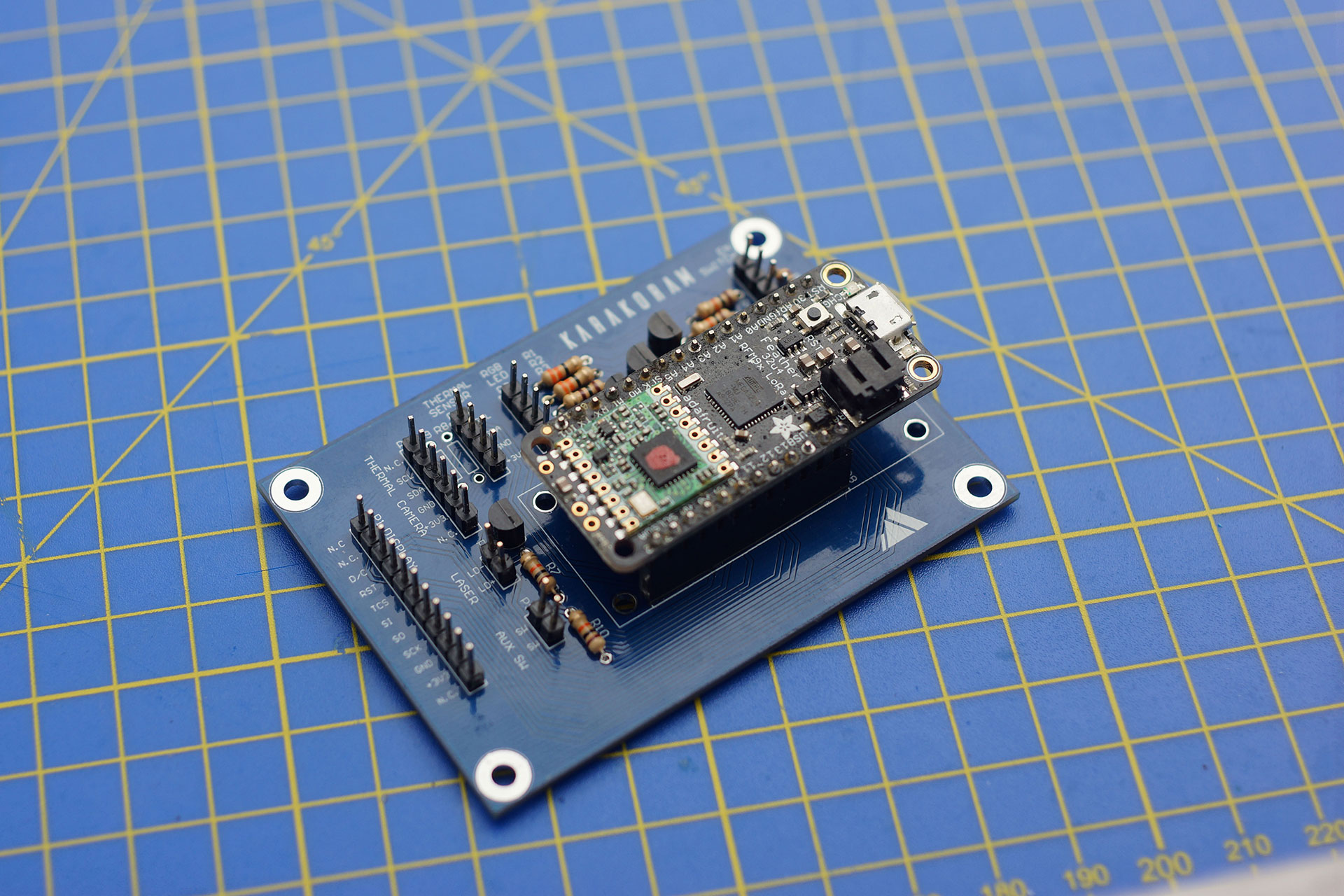
The Theia Thermometer was custom designed for this challenge. This included the industrial design, mechanical engineering, and the design of custom-built electronics and PCBs, manufactured in China by PCBWay.
The individual anonymous body temperatures data points captured by the Theia Thermometer are wirelessly transmitted over an embedded ultra-long-distance LoRa radio to the Theia Hub for interpretation and distribution to the national health service.
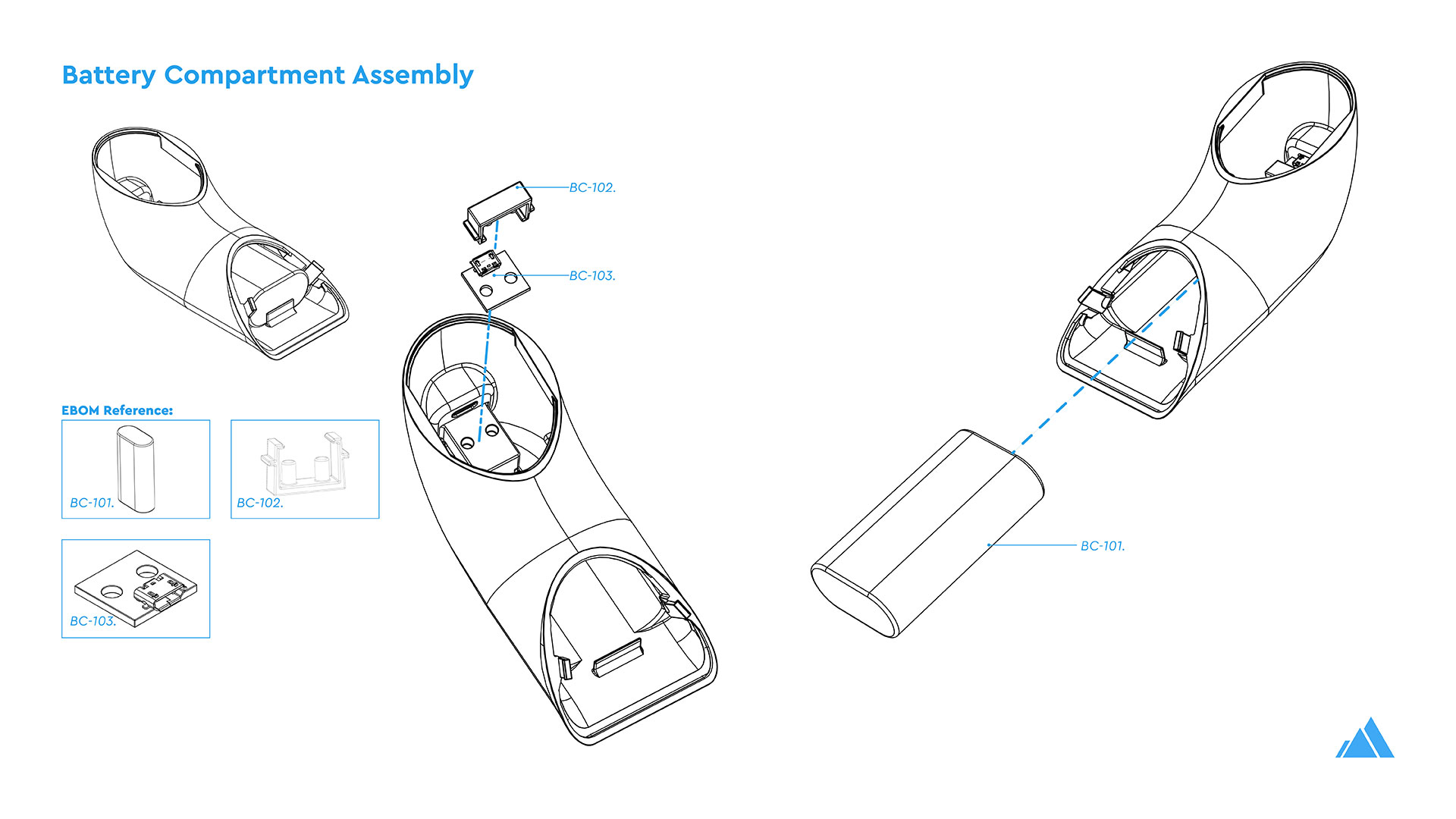
- Low-cost design using commercial-off-the-shelf components
- Designed around a commonly available Adafruit Feather 32u4 development board
- Easy production and on-site manufacture
- Can be assembled without screws or glue
- Clips together with innovative fastening features
- Long battery life (average 14-16 hrs)
- Elegant but rugged design (operational in any environment)
- Embedded low-power, ultra-long-distance 2km LoRa radio
Theia Hub

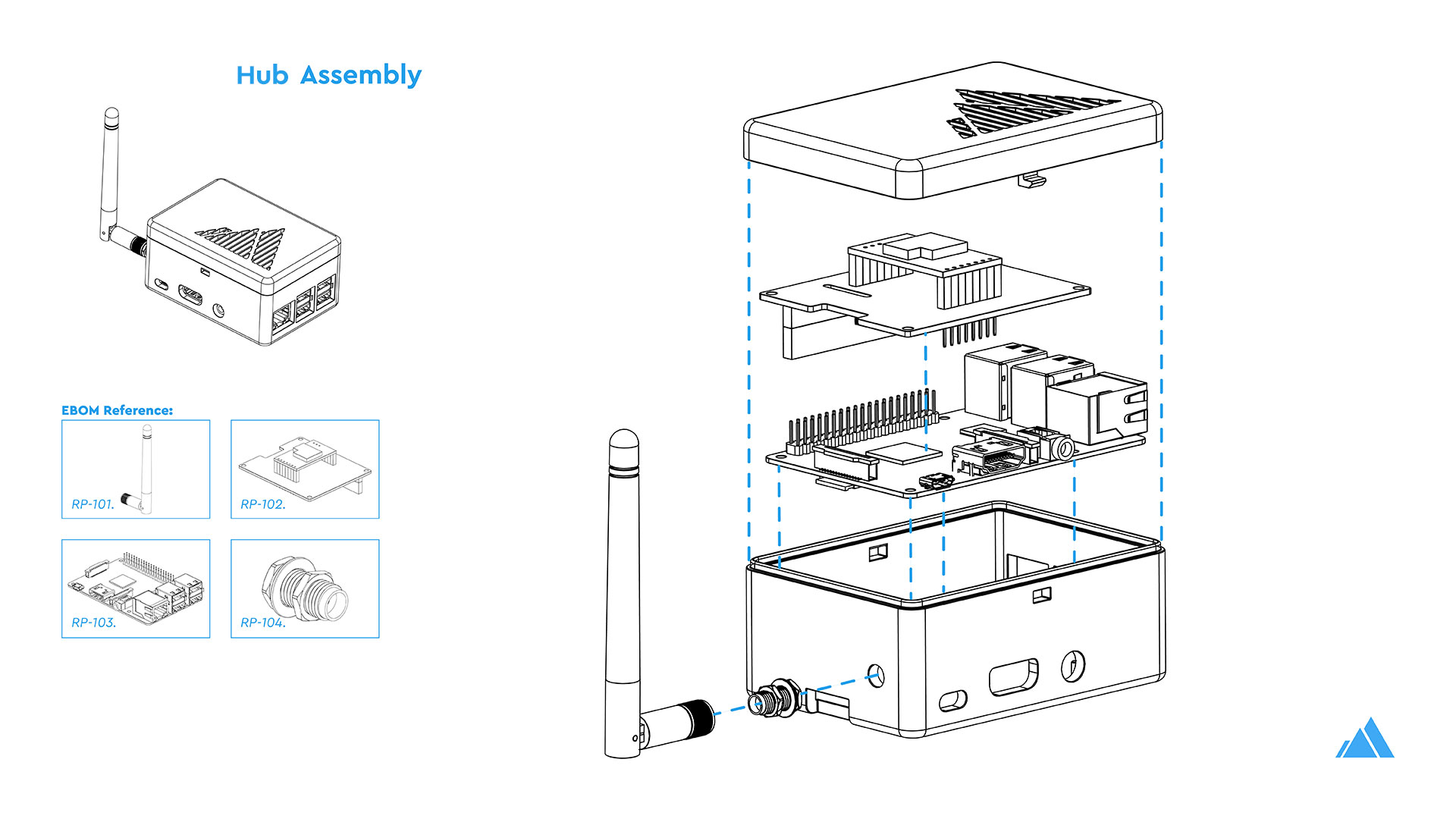
The Theia Hub listens for data transmissions in the particular, unlicensed, LoRa radio spectrum in each location and writes anonymous data points to a self-hosted InfluxDB database. The Hub interprets the data (currently limited in V1 to simple mean average calculations) and served by a Grafana self-hosted web front-end.
With the use of multiple Theia Thermometers and Theia Hubs, a developing country with limited healthcare services would have the minimum necessary real-time data on where average mean temperatures are increasing nationally. Project Theia offers the ability to intelligently distribute limited healthcare services without the need for established telecommunication networks (3G/4G/WiFi, etc.) or traditional track and trace methods.
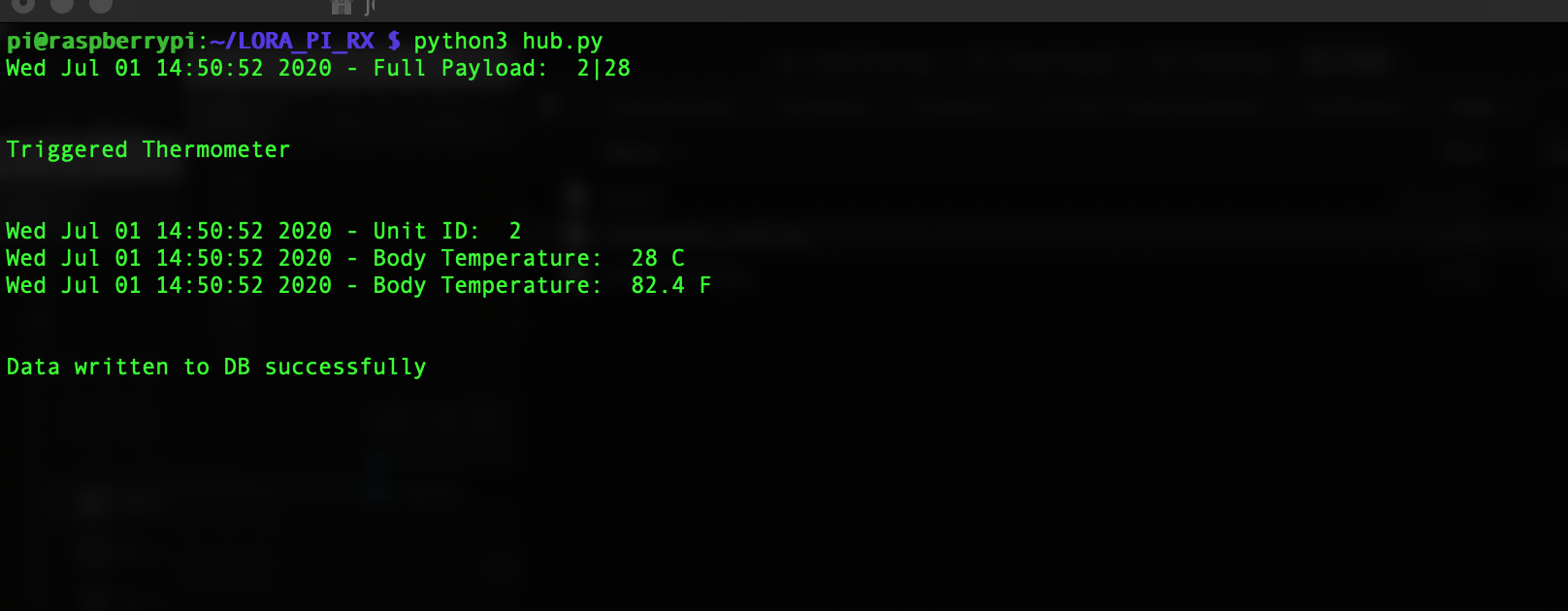
- Designed to listen / record & process submitted data points from any Theia Thermometer in the area (up to 2km radius).
- Wireless receiver via a LoRa radio chip
- Uses a python script to record data points to an InfluxDB database, as well as simple math based interpretations of the data
- Self-hosted Grafana web interface for the front-end
- Wireless consolidation of data points from the smart thermometers
- No requirement for Bluetooth, WiFi, 3G/4G, etc
Theia Dashboard
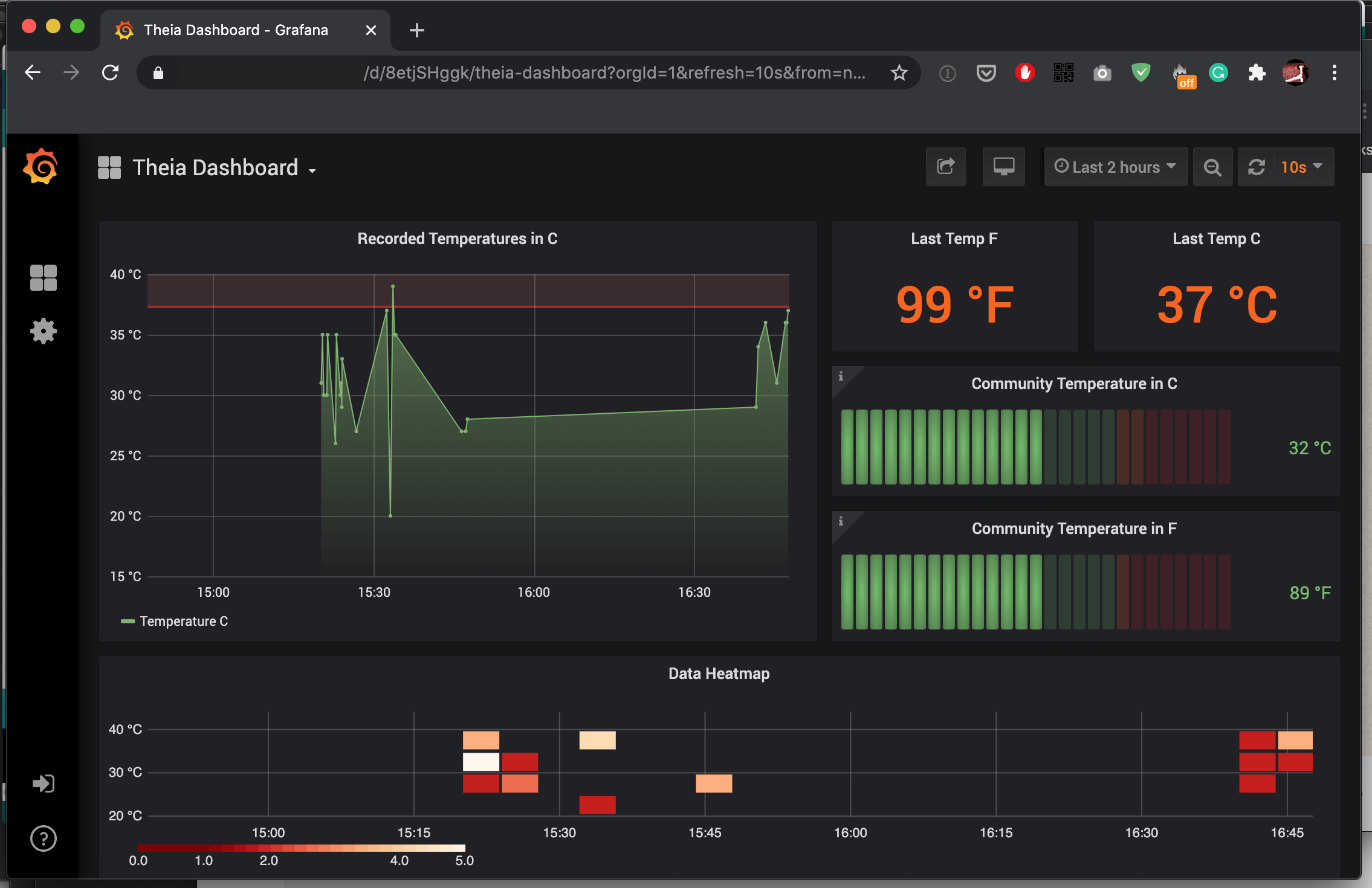
As discussed, contactless thermometers on their own, while useful placebos for emotional security during a pandemic, are primarily inaccurate for detecting COVID-19 due to the high number of other reasons that someone might have a fever. However, a sudden shift in the mean average temperature of a community body temperature would be an interesting metric for an outbreak of a highly infectious disease such as COVID-19. By looking for abrupt changes in the mean average body temperature of a village or community, the dashboard can automatically notify the national health service to deploy as needed.

Result

For those interested in building this platform a full build tutorial is available through our project writeup on Hackster.io.